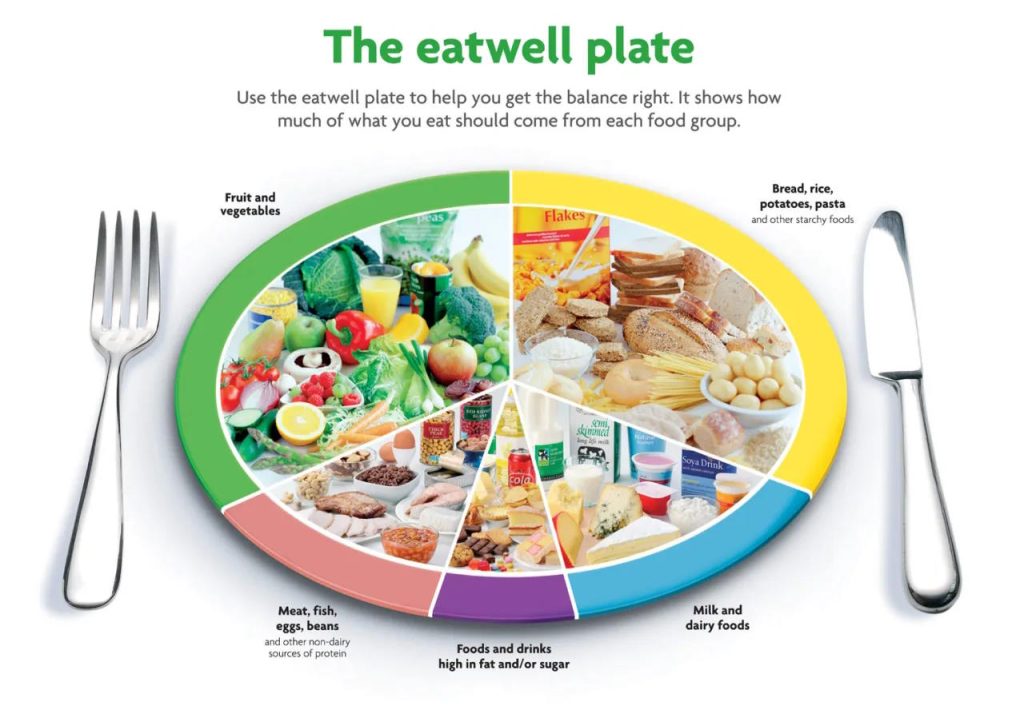
The Eatwell Plate, a dietary guideline endorsed by the European Parliament, has faced criticism, particularly for its emphasis on starchy foods, which some deem as “misguided.” This nutritional recommendation, officially termed the Eatwell Guide, was first introduced in 1983 and later updated by Public Health England. It outlines that meals should primarily consist of starchy carbohydrates such as potatoes, bread, rice, and pasta, accompanied by low or reduced-fat cheese and yogurt, and preferably unsaturated oils and spreads.
In contrast, prominent figures in the field, including cardiologist Dr. Aseem Malhotra, former Royal College of Physicians president Sir Richard Thompson, and nutritionist Sarah Macklin, advocate for a reevaluation of official dietary guidelines. They propose embracing a low-carbohydrate, Mediterranean diet, especially to combat type 2 diabetes. Dr. Malhotra argues that adherence to independent scientific evidence, diverging from current low-fat government guidelines, could substantially reduce the reliance on diabetes drugs and insulin, leading to significant NHS cost savings.
Sir Richard emphasizes the importance of addressing the calorie content in carbohydrates rather than solely focusing on fat, attributing the surge in diabetes to excessive carbohydrate consumption. Dr. Alison Tedstone, chief nutritionist at Public Health England, counters these arguments, asserting that high-fat diets often lead to increased calorie intake, contributing to weight gain and elevating the risk of heart disease, type 2 diabetes, and certain cancers. She underscores the recommendation for a balanced diet centered on starchy, high-fiber carbohydrates while minimizing saturated fats.
The debate is further fuelled by the success of the Low Carb Program developed by Diabetes.co.uk. Over nearly two years, this program has demonstrated a cost saving of £835 per person annually through diabetes medication deprescription alone. With over 270,000 participants, the program has showcased tangible results, including a 1.2% reduction in HbA1c, a seven percent average weight loss, and one in four individuals achieving remission or significant improvement in their type 2 diabetes.